Pelvic Pain in Men & Chronic Pelvic Pain Syndrome (CPPS) Treatment in New York City
What is Chronic Pelvic Pain Syndrome or CPPS?
CPPS Symptoms
CPPS Causes
Male Pelvic Pain & Chronic Pelvic Pain Syndrome Treatment
Pelvic Floor Therapy for Men
Pelvic Pain in Men
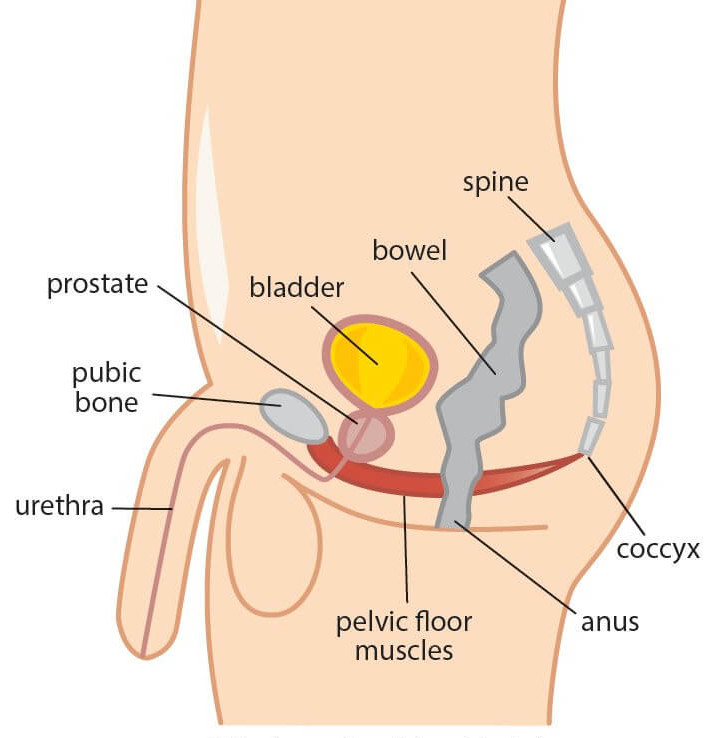
At some point in their lives men commonly experience pain in the pelvis or ‘pelvic pain’, a region of the body located between the abdomen and thighs encompassing the lower part of the abdomen, buttocks, groin and genitals.
Pelvic pain in men can be an indicator of multiple possible conditions. Pelvic pain in men can also have varying characteristics, be dull or sharp, precisely localized or spread throughout a large area. For example, kidney stones or pulled muscles can lead to sudden pelvic pain, whereas a urinary tract infection, bladder infection, or digestive problems can lead to a gradual onset of pelvic pain.
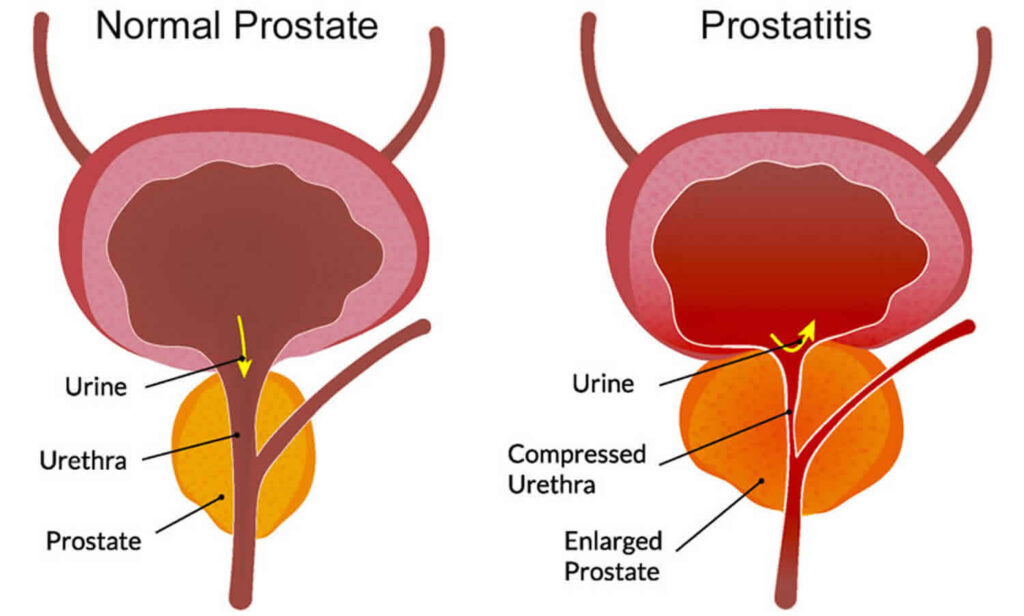
Often this pain is labeled as “prostatitis”, indicating inflammation of the prostate, which is a walnut-sized structure sitting in front of the rectum and under the bladder. In men younger than 50 years of age, prostatitis is the most common urologic diagnosis. While pelvic pain in men differs from that in women, an important commonality that they both share is that in most cases, pelvic pain in men is 100% treatable.
What is Chronic Pelvic Pain Syndrome (CPPS)?
Though the prostate is usually the source of pelvic pain in men, it’s important to know that the pain does not stem solely (or in some instances at all) from the prostate itself. Because the precise origin of the pain can be difficult and complex in pinpointing, The National Institute of Health (NIH) has attributed a more encompassing term for this pain, classifying it to be Chronic Pelvic Pain Syndrome (CPPS). Thus, chronic pelvic pain syndrome (CPPS) involves a set of disruptive symptoms, ongoing or repetitive pain episodes in the pelvic region, generally without bacterial infection or other causes that might explain the symptoms.
The National Institutes of Health classified Chronic Pelvic Pain Syndrome (CPPS) in men as follows:
- Chronic Pelvic Pain Syndrome I: sharp sudden pain, often accompanied with fevers and other signs of infection as well as bacteria in urine & treated in the standard way with antibiotics.
- Chronic Pelvic Pain Syndrome II: chronic or recurrent pelvic pain, accompanied with bacteria in urine, and the absence of signs of infections such as fevers & treated in the standard way with antibiotics.
- Chronic Pelvic Pain Syndrome III: chronic or recurrent pelvic pain with no presence of bacteria in urine and often subdivided into type A, when inflammatory cells are found in urine and type B, with that absence of inflammatory cells in urine. This is the most commonly seen type of CPPS seen in clinics. The most effective prescription for CPPS III type B, specifically, is pelvic floor physical therapy since it can directly treat the inflamed area.
- Chronic Pelvic Pain Syndrome IV: inflammatory cells present in urine or with the absence of any other symptoms and defined as prostate inflammation with no symptoms, and is only found incidental to other investigations.
By far the vast majority of all men diagnosed with Chronic Prostatitis / Chronic Pelvic Pain Syndrome are classified as having Category III, a common and debilitating condition affecting 5-12% of men.
Chronic pelvic pain syndrome is experienced in structures such as the muscles, nerves, & bony structures of the pelvis, abdomen and spine (Rees et al, 2015) that has been continuous or recurrent for at least six months – the minimum length of time for pelvic pain to be regarded as chronic (with the absence of urinary tract infection or other relevant cause).
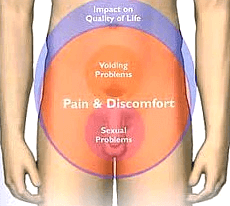
Chronic Pelvic Pain Syndrome (CPPS) Symptoms
Chronic Pelvic Pain Syndrome (CPPS) varies from person to person and is characterized by a wide range of symptoms and their severity, affecting the: pelvis, perineum, penis, scrotum, testes, rectum and lower back. One or multiple symptoms may be present and include:
- Pelvic pain: aching, burning, shooting, or itching sensation in the lower abdomen, buttocks, groin, and/or inner thighs.
- Genital pain: feeling pain in the testicles, scrotum, or general penis region.
- Perineal and/or anal/rectal pain (the perineal region includes the space between the genitals and anus).
- Urinary dysfunction: experienced as pain, urinary urgency, frequency, incomplete emptying, or dribbling of the urine.
- Any bowel dysfunction, bowel movement pain, constipation, bloating, incomplete emptying, gastrointestinal distress
- Sexual dysfunction: pain at any part of ejaculation (prior, during, after) or erectile dysfunction
- Pain with sitting, particularly in the perineum or the “sit bones”.
- Pain with exercise or daily movements, like squatting, cycling, situps, or heavy lifting.
Chronic Pelvic Pain Syndrome (CPPS) Causes
The precise cause of Chronic pelvic pain syndrome (CPPS) is not clearly understood but a number of factors may be involved such as:
- Excessive sitting: working a job that requires extended periods of sitting or activities like cycling and horseback riding.
- Surgical trauma: surgical operations of any kind in the region of the pelvis
- Orthopedic injuries: trauma to the lower body (for example, hernia)
- Structural dysfunction: hip or leg length discrepancies, any lower body structural issues..
- Over-exercise, or a rapid change of exercise routine.
- Excessive straining of bowel movement and chronic constipation.
- Sexually transmitted infections.
- It can even occur without an identifiable cause.
Male Pelvic Pain & Chronic Pelvic Pain Syndrome Treatment
Research indicates that men with chronic pelvic pain syndrome or chronic prostatitis experienced relief from pain after receiving pelvic floor physical therapy. This includes reduction in urinary symptoms and improvement in overall quality of life from application of manual techniques.
Research also concludes that a formalized pelvic floor therapy program of neuromuscular re-education of the pelvic floor muscles together with interval bladder training can provide significant and lasting improvement in reducing pain, urinary urgency and frequency in male patients with pelvic pain or chronic pelvic pain syndrome.
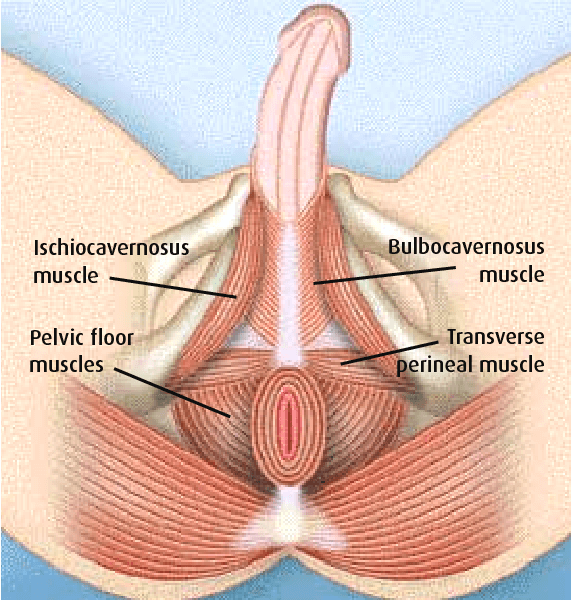
The pelvic floor is made up of 3 layers of muscles:
- functioning as a “sling” in support of the prostate, rectum, bladder, seminal vesicles and abdominal organs against gravity and any downward pressure
- stabilizing the connecting joints (pelvis & lower back) as one of four group of muscles making up our inner ‘core’.
- assist in bladder, bowel and sexual function.
Different from the muscles that you can see on the outside, these are mostly internal or inside the body. These muscles are vital to your daily functioning and movement and easily affected by sleep, stress, and other lifestyle factors.
The close relationship between the prostate and the muscle of the pelvic floor is well researched and understood. The prostate sits directly on these muscles and are all covered by connective tissue. The urethra extends down from the bladder through the prostate and external urinary sphincter, all within the muscular layer of the pelvic floor. Pelvic floor muscle tension or dysfunction can not only adversely affect the prostate and genitals themselves, but also the blood vessels, nerves, and fascia within the pelvis – producing broad regional pain and compromising the function of the urethra and anus. It should be noted muscles have great potential as “pain generators” and the fact is pain symptoms originate more from muscular tissue than any other source within the body. This is confirmed in context to male pelvic pain by 3 key research findings:
“Although the pain of chronic pelvic pain syndrome is poorly understood, nearly all clinicians agree that almost all chronic pelvic pain syndrome patients have some chronic tension and tenderness of the pelvic floor musculature. It is probable that these myofascial (sensitive muscle tissues) abnormalities contribute significantly to the pain of chronic pelvic pain syndrome.” – Nickel JC et al. Management of Men Diagnosed with Chronic Pelvic Pain Syndrome Who Have Failed Traditional Management. Reviews in Urology 2007; 9(2): 63-72. Source.
“A significant extraprostatic [outside the prostate] factor in generating pain in many men with chronic pelvic pain syndrome is pelvic floor spasm. This muscular spasm alone can produce and mimic the pain and lower urinary tract symptoms of chronic pelvic pain syndrome.” -Westesson KE and Shoskes DA. Chronic Prostatitis / Chronic Pelvic Pain Syndrome and Pelvic Floor Spasm: Can We Diagnose and Treat? Current Urology Reports 2010; 11: 261-264. Source.
“A muscle that is continuously contracting will ache. Nerves that pass through the pelvic floor may be compressed, and [blood] vessels to the penis and scrotum may be obstructed. Both mechanisms will lead to pelvic pain. … Repeated or chronic muscular overload can activate trigger points in the muscle.” – Fall M (chair) et al. Guidelines on Chronic Pelvic Pain. European Association of Urology 2008. Source.
Pelvic Floor Therapy for Men
Pelvic floor muscles contract and relax just as other muscles in the body – and as such are prone to dysfunction including tightness, weakness, spasms, and impaired coordination – all commonly leading to the symptoms mentioned above. Pelvic floor physical therapy can help reduce these symptoms and restore normal functioning of the pelvic floor/pelvic girdle region associated with pelvic pain in men including chronic pelvic pain syndrome.
Pelvic floor physical therapy provides a broad variety of techniques that are safe and effective for chronic pelvic pain syndrome or chronic prostatitis and can help with:
- Identifying sources of pain
- Providing strategies to resolve and manage pain
- Identifying patterns to prevent flare-ups of pain or symptoms (e.g., changing posture and pelvic alignment with painful sitting; dietary habit adjustments to better manage any painful bowel issues and prevent constipation)
- Properly rehabilitating muscles if there is muscle dysfunction or weakness
Physical Therapy Techniques include:
- Biofeedback: To help with pelvic floor musculature strengthening and relaxation.
- Manual therapy including internal and external manipulation of the abdominal musculature and pelvic floor (treating palpable tender points within a muscle & myofascial trigger point release).
- Therapeutic exercises to improve mobility/flexibility, promote range of motion, and strengthen weak muscles.
- As applied to the pelvic floor, manual compression techniques to reduce painful symptoms for those diagnosed with urgency-frequency syndrome & interstitial cystitis.
The information provided here is educational, not medical advice. If you are a man coping with pelvic pain and the symptoms of chronic pelvic pain syndrome and want to learn how pelvic floor physical therapy can be helpful and or explore your treatment options, please contact Dr. Helen Kim for a complimentary phone consultation. During your initial appointment, we will review your medical history. If your symptoms and history indicate pelvic floor dysfunction, you’ll receive a thorough external and internal musculoskeletal examination. Findings determine the optimal plan of care aimed to address your goals of eliminating, or at least managing, pelvic pain.
Reach me if I can answer any questions on physical therapy, serving you locally in New York City or anywhere online virtually through “telehealth“.
Sign up for Pelvic Health and Wellness Tips






