Pelvic Organ Prolapse Physical Therapy Treatment in New York City
Pelvic Organ Prolapse Stages
What are the Symptoms of Pelvic Organ Prolapse?
What causes a Pelvic Organ Prolapse?
Treatment for Pelvic Organ Prolapse
Physical Therapy for Pelvic Organ Prolapse in New York City
What is a Pelvic Organ Prolapse?
The uterus, bladder and rectum are organs within a woman’s pelvis that are held in place by a woman’s pelvic floor (a complex “hammock” of muscles, ligaments, and fibers that are attached to the bony anatomy of your pelvic region). Should these support structures become weakened, stretched, or torn due to trauma or childbirth, the pelvic organs (uterus, bladder and rectum) might drop, become herniated or bulge (prolapse) from their normal and natural position and into the vaginal canal. Scar tissue in the perineum and abdomen can contribute to pelvic organ prolapse due to increased soft tissue restrictions around the support structures. The pelvic organ can also protrude outside the vagina should the prolapse becomes severe enough. When one of the pelvic organs drop into the vaginal canal, it is referred to as a pelvic organ prolapse. It’s important to note more than one pelvic organ can prolapse simultaneously. With a pelvic prolapse the organs that can be involved include the bladder, urethra, uterus, vagina, and rectum.
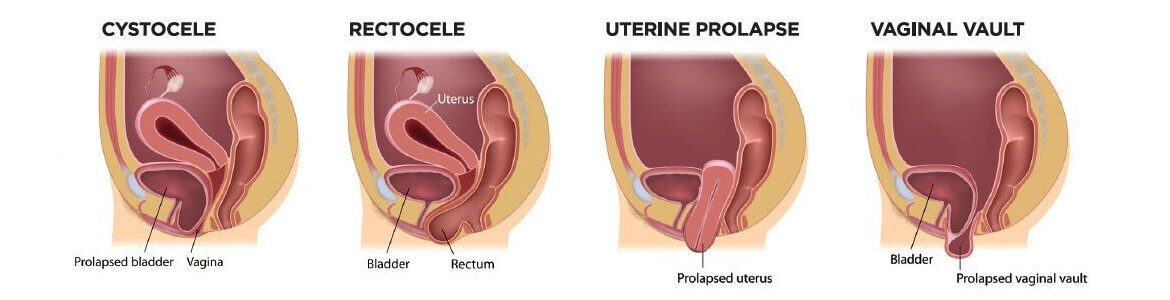
The 4 most common types of pelvic organ prolapses are:
- Anterior Prolapse: the bladder protruding into the front wall of the vagina
- Uterine Prolapse: the uterus protruding or sagging down into the vagina
- The top of the vagina slumping down – this occurs to some women after a hysterectomy
- Posterior Wall Prolapse: the rectum protruding forward into the back wall of the vagina
Pelvic Organ Prolapse Stages
When a woman has pelvic organ prolapse, the extent of the prolapse is described in the form of a stage. Assigning stages helps healthcare providers objectively characterize how large the protrusion or bulge of a prolapse is upon physical examination of the pelvis. There are 4 stages, with Stage 1 being the minimal amount of prolapse and Stage 4 being the largest degree of prolapse.
Staging of a pelvic organ prolapse is through clinical examination of the pelvis (no CT scans or MRIs are needed). There are numerous regions of the pelvis that are independently staged: the back vaginal wall, the front vaginal wall, and the top or apex of the vagina.
- Stage 1: Minimal prolapse – pelvic organs still supported by the pelvic floor muscles.
- Stage 2: Pelvic floor organs have begun to sag, but are still contained inside the vagina.
- Stage 3: Pelvic floor organs are sagging to, or slightly beyond the vaginal opening.
- Stage 4: Pelvic floor organs have fallen completely through the vaginal opening.
Pelvic floor physical therapy can be helpful in treating stages 1 or 2, along with pessaries (discussed later) in holding the organs in place. The most extreme circumstance, stage 4, is when pelvic organs push through the vaginal wall and are clearly visible outside the vagina.
For some women, experiencing even stage 1 of a pelvic organ prolapse can significantly alter their quality of life. They can have a feeling of heaviness or pressure in the vagina, constipation, and pain during sexual intercourse. It’s fairly common, with about 50% of women having some degree of prolapse in their lifetime. Fortunately , there are treatment options to explore that can significantly improve and in some cases, eliminate the symptoms of a pelvic organ prolapse . They include the use of pessaries—small medical devices of varying shapes that are inserted vaginally to provide structural support— or other types of tampon-like products, pelvic floor physical therapy, or in some cases, surgery.
What are the Symptoms of Pelvic Organ Prolapse?
Symptoms vary depending on the type and severity of the pelvic organ prolapse.
• Experiencing no symptoms at all is possible, only to discover you have a prolapse after a healthcare professional’s vaginal examination.
• The sensation of a lump ‘coming down’ is the most common symptom. You experience a backache, or a heavy or a dragging feeling inside your vagina. These symptoms seem worse at the end of the day or if you have been standing (or sitting) for a long time. Lying down seems to alleviate the symptoms.
• It’s possible a lump or bulge is visible, and you can feel it. Some women would have to manually push it back in to reduce the prolapse. If this is constant, it is best to get checked by your physician as the prolapse can become ulcerated or infected over time. A pessary or surgery would probably be recommended at this stage.
• Should a bladder prolapse into the vagina, it’s possible to have to urinate more frequently, experience difficulty urinating or the sensation your bladder is not completely emptying, experience leaking (urine) when laughing, coughing, or lifting heavy items, and or have an increase in urinary tract infections
• A rectocele, or a prolapsed rectum, can lead to constipation or incomplete bowel emptying, along with low back pain. Some women who have a rectocele may have to support the perineum or intravaginally splint in order to to allow stools to pass.
• You may experience a lack of sensation and or increased discomfort or pain during intercourse.
What causes a Pelvic Organ Prolapse?
Pelvic organ prolapse occurs when the pelvic floor weakens and can no longer firmly support the pelvic organs. Numerous factors can weaken your pelvic floor increasing the possibility of a pelvic organ prolapse. A major cause is damage to the pelvic floor’s muscles, ligaments, and nerves originating from the following:
• Pregnancy and childbirth are recognized as major factors weakening the supporting structures of the pelvic floor. About 1 in 3 women who have had a vaginal delivery experience some level of a pelvic organ prolapse. It may start during the pregnancy and continue into the postpartum period. A long labor and a difficult delivery, necessitating the use of forceps or vacuum, can contribute to a pelvic organ prolapse.
• Menopause, aging, and hormonal changes that further weakens the pelvic floor structures.
• Conditions causing repetitive and increased downward pressure on the pelvic floor like chronic cough, chronic constipation, obesity, heavy straining or lifting.
• The risk for pelvic organ prolapse can be inherited in some cases, such as diseases that affect the strength of connective tissue, e.g. Ehlers-Danlos syndrome and Marfan syndrome.
Treatment for Pelvic Organ Prolapse
It’s important to first say at the end of the day, decisions about your treatment will be based on which pelvic organs have prolapsed and how bad your symptoms are. Every patient’s history is unique and I am offering general education on approaches to the treatment of a pelvic organ prolapse.
As pelvic organ prolapse is due to weakened pelvic tissues along with weakened pelvic floor muscles, it’s sensible to keep your pelvic floor muscles healthy and strong – no matter your age. Be mindful a pelvic organ prolapse can effectively be treated without surgery, particularly in the early stages (stage 1 & 2) and when the prolapse is relatively mild. Just like any other muscles, pelvic floor muscles can be made stronger with the correct training techniques and properly executed exercises.
It’s also important to learn what factors contributed to or caused your pelvic organ prolapse and to make any necessary lifestyle changes to promote pelvic health. This might involve improving your diet (sufficient fiber and hydration to avoid constipation), losing weight, and practicing good bowel and bladder habits to avoid chronic straining when using the toilet. Perhaps a pessary fitting (usually a ring-like device inserted nonsurgically into your vagina) can help provide internal support for your pelvic organs. With the prolapsed organ supported in its normal position, many women experience relief from their symptoms from the use of a pessary ring.
For severe symptoms of pelvic organ prolapse, surgery is another treatment option. You can consult with a surgeon who specializes in pelvic floor conditions and see what the options are. But you might consider delaying having surgery if you’re planning to have more children as the strain of pregnancy and childbirth could enable the prolapse to return.
Physical Therapy for Pelvic Organ Prolapse in New York City
Physical therapy is recognized as a highly effective nonsurgical treatment for a pelvic organ prolapse. Research (Panman et al in 2016), demonstrated that with women aged 55 and older with symptomatic mild pelvic organ prolapse, pelvic floor muscle retraining resulted in a significant decrease in pelvic floor symptoms when compared to watchful waiting. Research also has shown that pelvic organ prolapse can be reduced by one grade with pelvic floor physical therapy. Source, here & here.
If it’s determined you’re experiencing a pelvic organ prolapse, you will benefit from a specialized physical therapy program in order to address the strength, flexibility, and endurance of your core and pelvic floor muscles. The goal of therapy is to reduce and alleviate symptoms, and prevent exacerbation of the prolapse. You will also be taught strategies and exercises to independently manage your condition.
Pelvic floor exercises, such as Kegel exercises, are known to help strengthen muscles and provide support for pelvic organs. Doing Kegel exercises is one of the best ways to mitigate the symptoms and prevent any further development of pelvic organ prolapse. Also, after childbirth, you should start performing regular pelvic floor exercises to strengthen the pelvic muscles. It’s helpful to return to your pre-pregnancy body mass index (BMI) about 1 year after giving birth since this reduces your risk for pelvic organ prolapse.
If you or someone you know is experiencing any of the symptoms of a pelvic organ prolapse, don’t delay in seeking help through pelvic floor physical therapy. There is no need for embarrassment or suffering in silence. As a physical therapist I can help guide treatment for pelvic organ prolapse as part of a comprehensive program, incorporating pelvic floor techniques, self care, and exercises, and collaborating with your physicians or surgeons for the best care possible.
The information provided is educational, not medical advice. If you are someone dealing with a potential pelvic organ prolapse and want to learn how pelvic floor physical therapy can be helpful and or explore your treatment options, please consider contacting me, Dr. Helen Kim, for a complimentary phone consultation.
Reach me if I can answer any questions on physical therapy, serving you locally in New York City or anywhere online virtually through “telehealth“.
Sign up for Pelvic Health and Wellness Tips