5 Reasons For Painful Sex
About 20 percent of women in the US experience dyspareunia, which is defined as persistent and current painful sexual intercourse, at some point in their lives. It can contribute to feelings of depression and anxiety and have a significant impact on intimacy and personal relationships. Hormonal changes, pelvic diseases, and physical/ emotional trauma can cause dyspareunia. It can be described as an entry and/or a deep pain in the pelvis with penetration. Pelvic floor physical therapy can help treat the soft tissue and muscles that become affected over time from these conditions.
What is the Pelvic Floor?
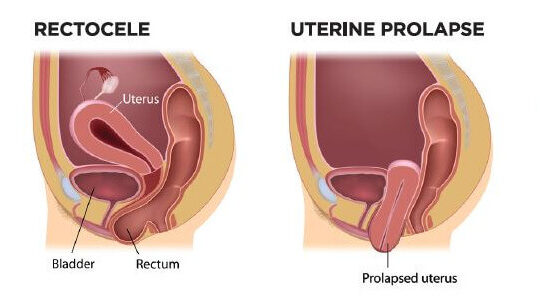
The pelvic floor is comprised of three layers of muscles that line the bottom and the sides of the pelvis. The deepest layer partially forms the walls of the pelvis and a hammock-like structure that supports the pelvic organs, such as the uterus, bladder, and rectum. This sling attaches to the pubic bone and tailbone, The outermost layers of the pelvic floor located in the vulvar region contribute to sexual function and urinary continence.
Trauma to these muscles and the surrounding area, including skin and connective tissue, will lead to scarring and pelvic floor dysfunction, such as urinary or fecal incontinence, pain, hypersensitivity of the area, and difficulty relaxing or contracting the pelvic floor muscles.
What are some causes of Dyspareunia?
- Menopause. About half of postmenopausal women suffer from painful sexual intercourse. During menopause, the drop in estrogen levels can lead to vulvar atrophy and dryness. This leads to the superficial tissues of the vagina getting fragile and can get irritated and tear with friction. Topical creams, vaginal moisturizers, and lubricants are useful in treating the effects of menopause by improving the health and texture of the vulvar tissue, maintaining lubrication and reducing irritation.
- Childbirth and Breastfeeding. Dyspareunia is common in 40-50% of women after delivery at 3 months postpartum. Studies show that severe perineal tears sustained during delivery or episiotomies are correlated with persistent dyspareunia. You may feel more superficial entry pain, such as a burning or stinging sensation with intercourse. If you are breastfeeding, you can also develop vaginal dryness due to the decreased levels of estrogen in your body. Using vaginal moisturizers and lubricant products frequently can help as well as increased water intake throughout the day. You can also incorporate certain types of food with good fats into your diet, such as avocados.
- Pelvic Conditions and Disorders. Common pelvic conditions linked to chronic pelvic pain are Endometriosis, Interstitial Cystitis, and Pelvic Congestion. Endometriosis is a disease where endometrial like tissue grows outside of the uterus, most often in the abdominal and pelvic regions. This can lead to painful adhesions and scar tissue around the uterus, bladder, rectum, ovaries, and fallopian tubes. Muscles of the hip, abdomen, and pelvic floor will become tight and painful in the area of the lesions. Interstitial cystitis, or bladder pain syndrome, is a condition related to chronic pelvic pain > 6 months, persistent urge to urinate and temporary relief with urination, and discomfort or pain related to bladder filling. There are specific trigger points in the pelvic floor muscles that can trigger pelvic pain, urinary frequency, hesitancy, and painful intercourse. These symptoms can also be exacerbated by certain liquids, foods, and stress. Pelvic congestion syndrome is associated with abnormal enlargement of veins in the pelvis usually diagnosed in women of childbearing age, leading to congestion of the varicose veins around the ovaries and chronic pelvic pain. It can also occur with endometriosis, uterine fibroids, pregnancy and increased estrogen levels, or hormonal dysfunction. Other risk factors include multiple pregnancies and polycystic ovaries. Pain is generally the worst in the upright position and during or after sexual intercourse.
- Physical or Emotional Trauma. Over time, our bodies react and adapt to physical and emotional trauma, leading to tightness of the pelvic floor, chronic pain, and increased sensitivity/ decreased threshold to pain. Past and ongoing emotional trauma can contribute to an upregulation or central sensitization of the nervous system. Over time, pain signals sent to the brain by your muscles become progressively amplified and your body will start to perceive these signals as harmful.
- Abdominal Surgery. Undergoing a total abdominal hysterectomy or a cesarean results in pain, scarring, and adhesions of the abdominal wall. The abdomen can feel very restricted and affect breathing and movement. In addition to the abdominals becoming weakened, the pelvic floor can also become tight and weak, inhibiting or making intercourse painful.
How can Pelvic Floor Physical Therapy help?
Pelvic floor physical therapy includes stretching of tissues and scars with internal and external techniques to promote mobility and decrease pain. Biofeedback units with internal vaginal sensors may be used if you have difficulty activating or relaxing the pelvic floor muscles. Exercises that increase awareness of pelvic floor muscles are also incorporated, such as with breathing and relaxation techniques, stretches for the pelvic floor, and exercises to correct pelvic and spinal alignment and to promote stability of these structures.
Because consistency is key to a successful outcome, you will also be instructed in a home exercise program. You may also be advised to also use tools such as dilators, pelvic wands, and internal units to continue self treatment in between your sessions. A bladder and food diary is also helpful if you have urinary urgency, frequency, or bladder pain. This will help your physical therapist identify certain triggers and help modify your diet and voiding pattern.
Reach me if I can answer any questions on physical therapy, serving you locally in New York City or anywhere online virtually through “telehealth“.
Sign up for Pelvic Health and Wellness Tips